The Health History Questionnaire serves a similar purpose to the Annual Physical Examination form by collecting detailed information about an individual's medical background. It typically includes sections for personal information, medical history, current medications, allergies, and family medical history. Both documents aim to ensure that healthcare providers have a comprehensive understanding of a patient's health status before conducting an examination or treatment.
The Patient Intake Form is another document that shares similarities with the Annual Physical Examination form. This form is often used in medical offices to gather essential information from new patients. It includes sections for personal details, insurance information, medical history, and current medications. Like the Annual Physical Examination form, it seeks to streamline the process of obtaining relevant health information prior to a medical appointment.
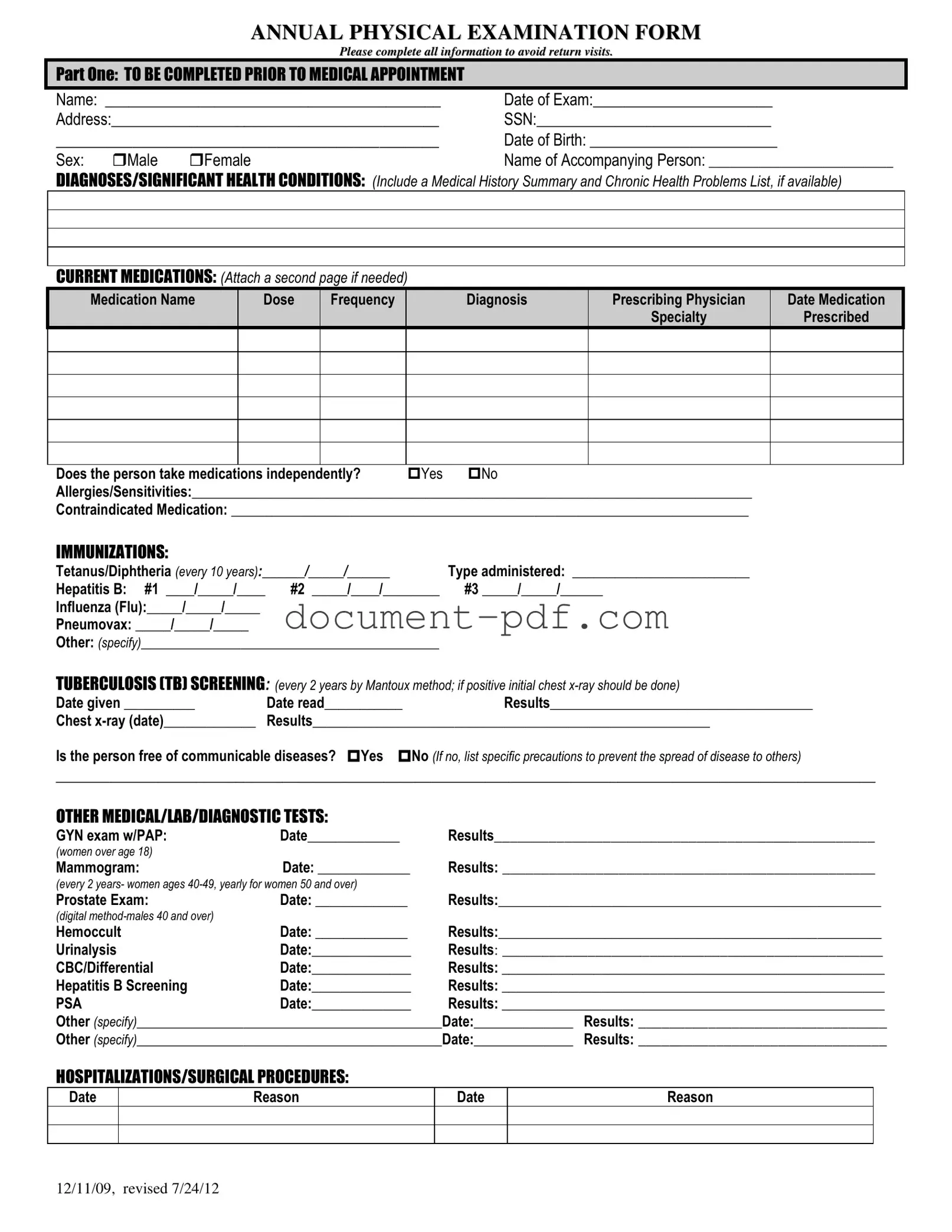
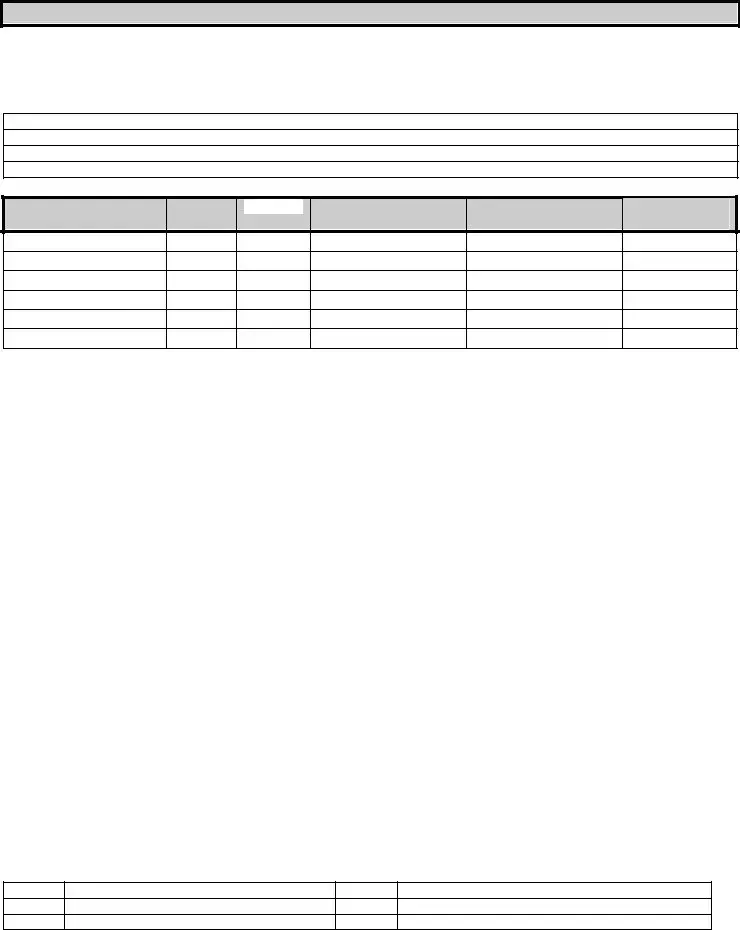
The Medication Reconciliation Form is closely related to the Annual Physical Examination form, particularly in its focus on current medications. This document is used to compare a patient's medication list against their current prescriptions to identify any discrepancies or potential interactions. Both forms emphasize the importance of accurate medication information for safe and effective healthcare delivery.
The Immunization Record is another document that parallels the Annual Physical Examination form. It tracks a patient's vaccination history, including dates and types of immunizations received. Both documents play a crucial role in ensuring that individuals are up to date on necessary vaccinations, which is vital for preventive health measures.
The Lab Test Requisition Form is similar to the Annual Physical Examination form in that it specifies tests that need to be performed based on a patient's health status. This form typically includes patient information, the specific tests ordered, and any relevant clinical information. Both documents are essential for guiding healthcare providers in assessing a patient's health through diagnostic testing.
The Consent for Treatment Form is another document that serves a similar function to the Annual Physical Examination form. It ensures that patients understand and agree to the procedures and examinations they will undergo. Both documents are critical for establishing clear communication between patients and healthcare providers, fostering informed consent.
The Medical Release Form is akin to the Annual Physical Examination form in that it allows healthcare providers to share a patient’s medical information with other parties, such as specialists or insurance companies. Both documents facilitate the flow of essential health information, which is vital for coordinated care and treatment planning.
For individuals looking to prepare their legal documents, the Last Will and Testament serves a similar purpose to the Annual Physical Examination form by ensuring that important aspects of one’s life are documented comprehensively. It emphasizes the significance of clear instruction regarding asset distribution after death, providing assurance that one’s wishes will be respected. For more information on how to create your Last Will and Testament, you can visit pdfdocshub.com/.
The Advance Directive Form shares similarities with the Annual Physical Examination form by addressing a patient's preferences for medical treatment in the event they are unable to communicate their wishes. Both documents focus on the patient's health and well-being, ensuring that their values and preferences are respected in medical decision-making.
The Follow-Up Appointment Form is another document that is similar to the Annual Physical Examination form. It is used to schedule and confirm subsequent visits based on the findings from the initial examination. Both documents aim to enhance continuity of care by ensuring that patients receive appropriate follow-up for any identified health concerns.
Finally, the Chronic Disease Management Plan is closely related to the Annual Physical Examination form. This document outlines a strategy for managing ongoing health conditions, including medications, lifestyle changes, and regular monitoring. Both documents emphasize proactive health management to improve patient outcomes and quality of life.