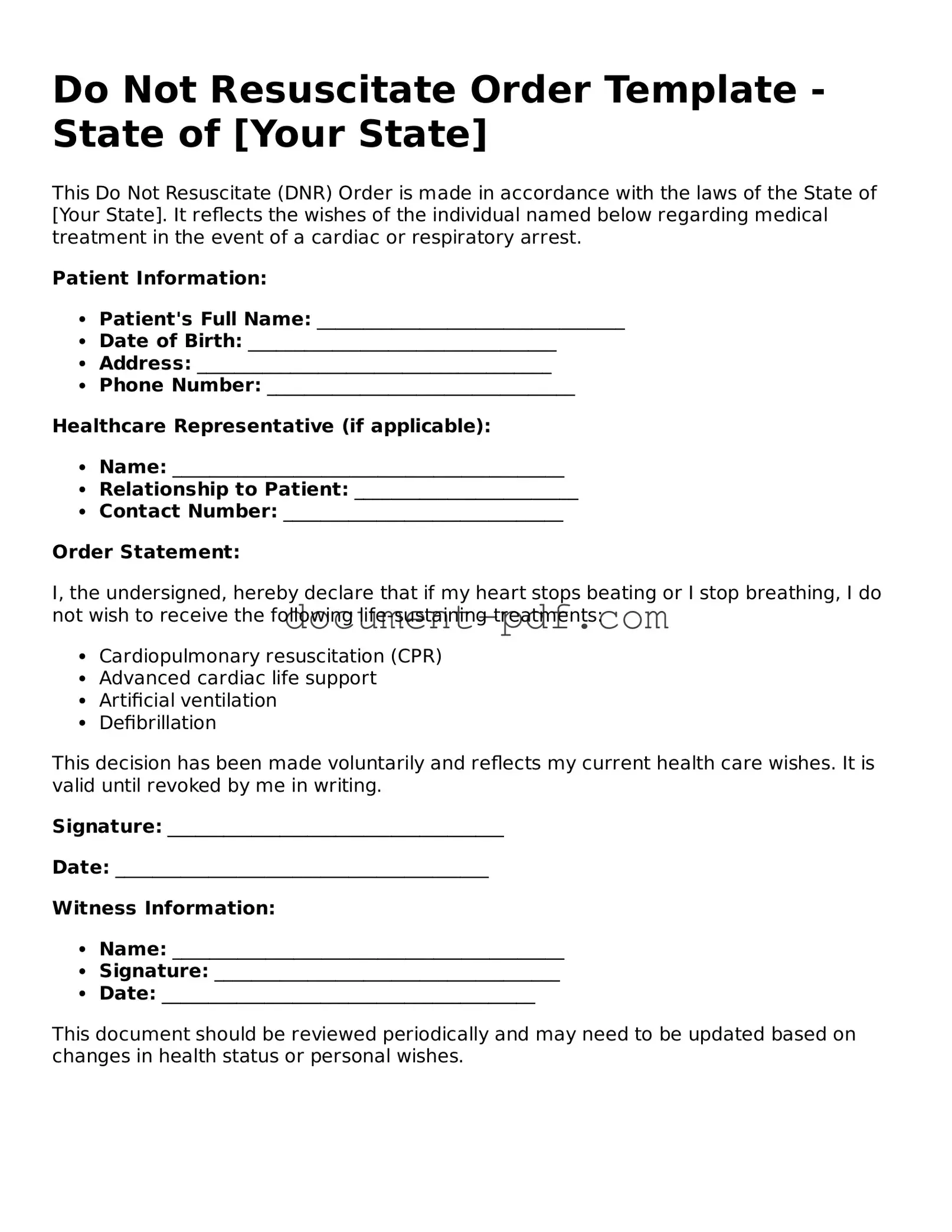
Attorney-Approved Do Not Resuscitate Order Document
A Do Not Resuscitate (DNR) Order is a legal document that allows individuals to refuse resuscitation efforts in the event of cardiac arrest or respiratory failure. This form is an important tool for patients who wish to have control over their medical treatment preferences, particularly in end-of-life situations. Understanding its implications can help ensure that a person's wishes are respected during critical moments.
If you are considering completing a DNR Order, please click the button below to begin the process.
Access Do Not Resuscitate Order Editor Here
Attorney-Approved Do Not Resuscitate Order Document
Access Do Not Resuscitate Order Editor Here
Finish the form without slowing down
Edit your Do Not Resuscitate Order online and download the finished file.
Access Do Not Resuscitate Order Editor Here
or
Click for PDF Form