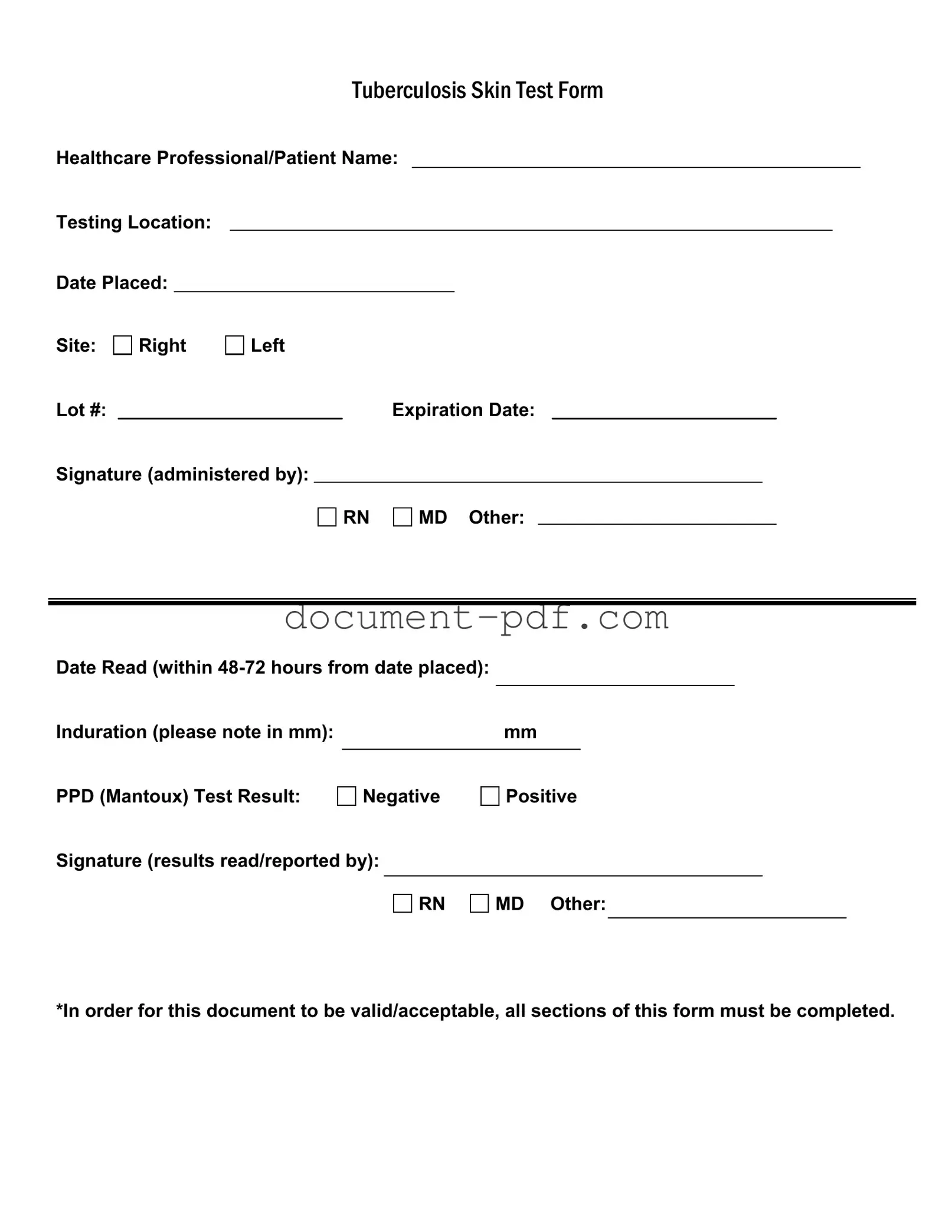
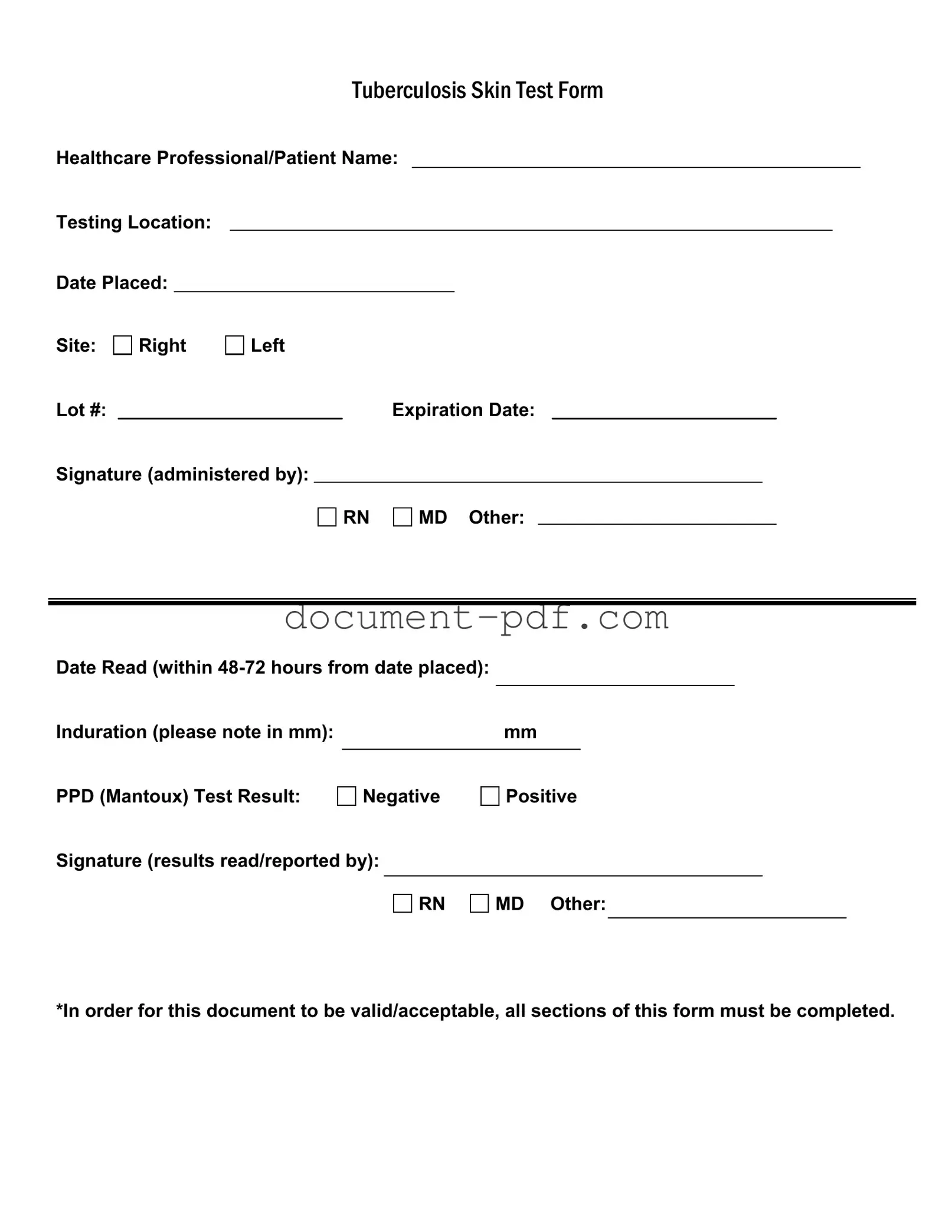
The Tuberculosis (TB) Test form shares similarities with the Vaccination Record. Both documents serve as official records of medical procedures performed on an individual. They require essential information such as the healthcare professional's name, the date the procedure was administered, and the location of the administration. Furthermore, each document includes a section for the healthcare provider's signature, which validates the information presented. The Vaccination Record, like the TB Test form, must be completed in full to ensure its acceptance by schools, employers, and healthcare facilities.
When considering your legal authority, the importance of understanding the comprehensive General Power of Attorney document cannot be overstated. This form not only enables a designated individual to manage your affairs but also ensures that your wishes are respected in various situations. Filling out the form accurately is crucial for maintaining your financial and legal interests effectively.
Another document akin to the TB Test form is the Medical Clearance Form. This form is often required by employers or educational institutions to verify an individual's health status before participation in certain activities. Similar to the TB Test form, it includes sections for the healthcare provider’s details, the date of the assessment, and a signature. Both documents aim to confirm that an individual is free from communicable diseases or other health issues that may pose a risk to others, thus ensuring public safety.
The Health Assessment Form also bears resemblance to the TB Test form. This document is commonly utilized in various healthcare settings to gather comprehensive health information about a patient. It typically includes details such as the patient's medical history, current medications, and recent test results. Like the TB Test form, the Health Assessment Form requires the signature of a healthcare professional to authenticate the information provided. Both forms are critical in establishing a patient's health status and guiding further medical decisions.
Lastly, the Physical Examination Report is another document similar to the TB Test form. This report is often required for sports participation, employment, or school enrollment. It includes vital information about the individual's physical health, including any tests performed, such as the TB test. Both documents require detailed information about the individual and the healthcare provider's signature, ensuring that the data is credible and reliable. The Physical Examination Report and the TB Test form both play essential roles in safeguarding public health by documenting the health status of individuals.