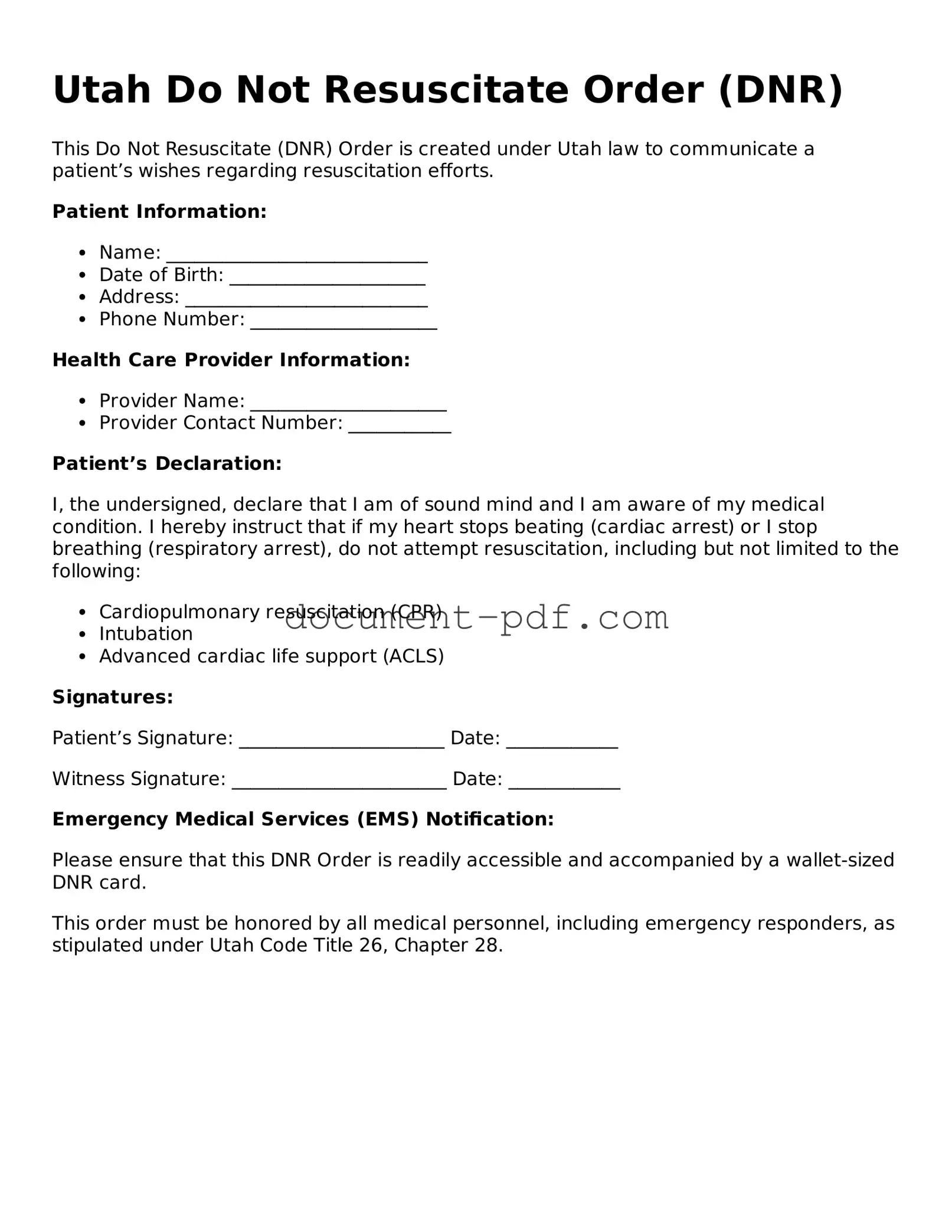
Attorney-Verified Utah Do Not Resuscitate Order Template
A Do Not Resuscitate Order (DNR) form in Utah is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. This form ensures that healthcare providers respect a person's decision not to receive cardiopulmonary resuscitation (CPR) or other life-saving measures. Understanding the implications of a DNR order is essential for making informed healthcare decisions.
To take the next step in expressing your wishes, please consider filling out the form by clicking the button below.
Access Do Not Resuscitate Order Editor Here
Attorney-Verified Utah Do Not Resuscitate Order Template
Access Do Not Resuscitate Order Editor Here
Finish the form without slowing down
Edit your Do Not Resuscitate Order online and download the finished file.
Access Do Not Resuscitate Order Editor Here
or
Click for PDF Form